doi: 10.4103/1673-5374.244781. Evidence on neuroprotective properties of coenzyme Q10 in the treatment of glaucoma
Affiliations
PMID:
30530997
PMCID:
PMC6301180
DOI:
10.4103/1673-5374.244781
The retina is one of the most metabolically active tissue
in the body and requires an accurate regulation of the energy
production. In this regard, mitochondria play a central role providing
energy supply through oxidative phosphorylation. Adenosine triphosphate
is generated by the electron transport chain complexes located within
the cristae folds of the inner mitochondrial membrane. Moreover,
mitochondria regulate a number of essential processes for neuronal
functions including metabolic balance, intracellular calcium
homeostasis, production of reactive oxygen species, and apoptotic
signalling. Experimental studies have shown that RGCs death in glaucoma
is an extremely complex process triggered by different molecular
mechanisms (Nucci et al., 2018). Due to peculiar structural and
energetic request, it is not surprising that RGCs are acutely vulnerable
to mitochondrial dysfunction (Lee et al., 2011; Ito and Di Polo, 2017),
which may increase their susceptibility to glaucoma-driven pathological
factors
(Figure 1).
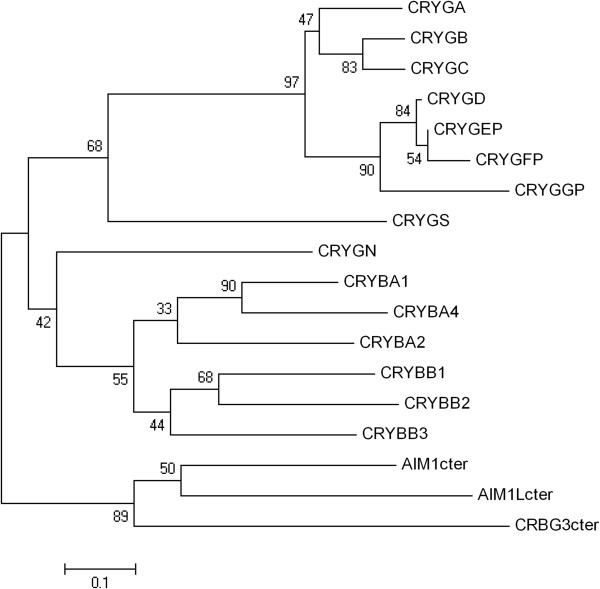
Main mechanisms of action of coenzyme Q10 (CoQ10).It has free radical
scavenging property that prevents deoxyribonucleic acid (DNA) damage,
has a fundamental role in cellular bioenergetics and a specific
antiapoptotic activity by directly maintaining mitochondrial
permeability transition pore (MPTP) in the closed conformation. The specific loss of RGCs is a common feature of
mitochondrial diseases (Lee et al., 2011). Indeed, inherited
mitochondrial defects are associated with a number of optic neuropathies
including Leber’s hereditary optic neuropathy and autosomal dominant
optic atrophy, but also with more severe central nervous system (CNS)
involvement in many other syndromic mitochondrial diseases, which are
characterized by selective RGC death (Carelli et al., 2009; Lee et al.,
2011; Ito and Di Polo, 2017).
The selective loss of neuronal populations and the
cell damage pattern in glaucoma also resemble those of other
neurodegenerative diseases (Nucci et al., 2016, 2018; Mancino et al.,
2018a, b) and increasing evidence supports a causative role of the
glutamate-induced excitotoxic mechanism in RGCs loss in in vitro and in vivo
experimental conditions (Nucci et al., 2007). Several free radical
scavengers and/or agents, that ameliorate mitochondrial function, have
been candidate as treating agents to prevent cell death in various
neurodegenerative conditions, such as Alzheimer’s disease and Parkinson,
and glaucoma (Spindler et al., 2009; Ahmadinejad et al., 2017). CoQ10
is both a ubiquitous free radical scavenger and a recognised electron
transporter in complexes I, II, and III of mitochondrial respiratory
chain. CoQ10 is an important antioxidant and has a fundamental role in
cellular bioenergetics. This led to consider glaucoma as a
neurodegenerative disease and promoted clinical studies on new
neuroprotective strategies not only targeted to IOP reduction (Nucci et
al., 2016, 2018).
Interestingly, increasing evidence indicates that
age-related mitochondrial defects play a central role in the
pathogenesis of glaucoma (Nucci et al., 2007; Russo et al., 2008, 2009;
Lee et al., 2014). Levels of CoQ10 in the human retina have been
reported to declines with age (Qu et al., 2009). In this regard, it is
well known the existence of a link between older age and the prevalence
of glaucoma, thus suggesting a possible increased vulnerability of RGCs
in glaucomatous neurodegeneration due to a lack of CoQ10 in older age
(Bhagavan and Chopra, 2006; Lee et al., 2014).
This opens new opportunities of investigation for
the development of novel neurotherapeutic agents for the treatment of
glaucoma and other major retinal pathologies (Russo et al., 2008, 2009;
Zhang et al., 2017).
CoQ10 poor aqueous solubility (Fato et al., 2010)
and low bioavailability, partially due to the interactions with the
multi-drug efflux pump P-glycoprotein expressed in both corneal
epithelial cells and RGCs, have limited the development of topically
active formulations of this molecule (Davis et al., 2017). To enhance
the topical delivery and pharmacological effects of CoQ10, the
co-administration with a P-glycoprotein inhibitor, such as
D-α-Tocopherol polyethylene glycol 1000 succinate (TPGS), has been
proposed (Davis et al., 2017). Interestingly, it has been successfully
demonstrated both in vitro and in vivo
mitochondrial-mediated neurotoxicity models that twice daily topical
instillation of CoQ10/TPGS micelles was found to be significantly
neuroprotective against RGCs loss than TPGS alone. The findings, in
agreement with previous work, also suggest that the antioxidant activity
of TPGS alone was insufficient to protect an immortalised neuronal cell
line from insults generating mitochondrial oxidative stress, such as
dimethyl sulfoxide and paraquat (Davis et al., 2017).
Topical ocular administration, in a model of high
IOP–induced transient ischemia in rat, of CoQ10 0.1% + vitamin E (Vit E)
0.5% showed the ability to minimize DNA fragmentation and retinal cell
apoptosis (Nucci et al., 2007) (Figure 1).
This study confirmed, for the first time, that, during the reperfusion
phase, the ischemic insult induces a significant increase of glutamate
with consequent RGCs apoptosis. Thus, providing evidence of the
usefulness of CoQ10 as a neuroprotective agent. In these conditions,
administration of CoQ10 prevents glutamate increase, minimizing RGCs
death in rats. It is plausible that the CoQ10 free radical scavenging
mechanism may have a minor role in this process and that CoQ10 ability
to restrains extracellular glutamate accumulation, may reduce the
harmful effect of ischemia/reperfusion on mitochondrial energy
metabolism and, accordingly, on the glutamate transporters function,
preventing RGC apoptosis in the rats (Nucci et al., 2007). Excessive
activation of glutamate receptors via the excitotoxic cascade leads to
the MPTP formation and release of a proapoptotic factor, the cytochrome
C, from the mitochondrial intermembrane space into the cytosol.
Remarkably, CoQ10 inhibits this cascade by maintaining MPTP in the
closed conformation, preventing apoptosis (Papucci et al., 2003).
The main concern about the topical administration
was the concentration of CoQ10 at the retinal and vitreal level reached
after the instillation of the eye drops. In this regard, it has been
reported that when CoQ10 in association with Vit E eye drops are
topically applied to the cornea, CoQ10 reaches the retina, substantially
increasing local CoQ10 concentration and protecting retinal layers from
apoptosis, in a mouse model of kainate-induced retinal damage. In
addition, patients undergoing pars plana vitrectomy, who were
administered CoQ10 in association with Vit E eye drops 1 hour before
surgery, showed the presence of CoQ10 in the collected vitreous samples,
thus confirming the ability of CoQ10 to reach the posterior ocular
tissues (Fato et al., 2010; Lulli et al., 2012).
Oral administration of CoQ10 has also been
reported to be neuroprotective in neurodegenerative diseases, as well as
in cardiovascular diseases. CoQ10 supplementation has been reported to
increase plasma CoQ10 concentrations, and the safety of high doses of
orally-ingested CoQ10 over long periods has been well documented also in
humans (Bhagavan and Chopra, 2006). Interestingly, it has been reported
that CoQ10 is taken up by all tissues, including heart and brain
mitochondria. This finding, together with growing evidence indicating
that CoQ10 is neuroprotective in RGCs against IOP in vivo and in vitro,
as well as against oxidative stress and excitotoxicity, suggests that
CoQ10 could also be taken up by the retina and lead to a beneficial
effect in glaucomatous retina (Lee et al., 2014). In a recent study on
preglaucomatous DBA/2J and age-matched control DBA/2J-Gpnmb+
mice, diet supplementation with CoQ10 for 6 months was tested to assess
the effects on glutamate excitotoxicity and oxidative stress-mediated
RGC degeneration (Lee et al., 2014). Intriguingly, CoQ10 endorsed RGC
survival, preserved the axons in the optic nerve head, and inhibited
astroglial activation by reducing glial fibrillary acidic protein
expression in the retina and optic nerve head of glaucomatous DBA/2J
mice. Interestingly, CoQ10 significantly blocked the upregulation of
N-methyl-D-aspartate receptor 1 and 2A, as well as of superoxide
dismutase-2, heme oxygenase-1 protein expression in the retina of
glaucomatous DBA/2J mice. Moreover, CoQ10 was able to prevent cell
apoptosis by reducing Bax protein expression or by enhancing
phosphorylated Bad protein expression. mtDNA content and mitochondrial
transcription factor A/oxidative phosphorylation complex IV expression
in the retina of glaucomatous DBA/2J mice were also preserved by CoQ10
supplementation. This suggest that CoQ10 may have a beneficial potential
for ameliorating glutamate excitotoxicity and oxidative stress mediated
glaucomatous neurodegeneration in the retina (Lee et al., 2014).